Intestinal resection is a significant surgery that can save lives. It’s essential for patients and their families to understand what it involves. This knowledge helps them prepare and manage outcomes better. According to recent data, over 250,000 intestinal resection surgeries are performed annually in the U.S. alone. Understanding these procedures is crucial, especially for those with digestive health issues.
What is Intestinal Resection?
Intestinal resection, often called enterectomy or colectomy, refers to the removal of a section of the intestines. This surgery is vital for treating certain diseases of the bowel. There are two main types: removing parts of the small intestine (small bowel resection) and removing parts of the large intestine (large bowel resection).
There are different procedures under intestinal resection: – Duodenectomy: Removes part of the duodenum, the first section of the small intestine. – Jejunectomy: Focuses on the jejunum, the midsection of the small intestine. – Ileectomy: Targets the ileum, the latter part of the small intestine. – Colectomy: Involves removing part or all of the large intestine.
Each type addresses specific conditions and symptoms, improving patient health when medications or other treatments fall short.
How is Intestinal Resection Surgery Performed?
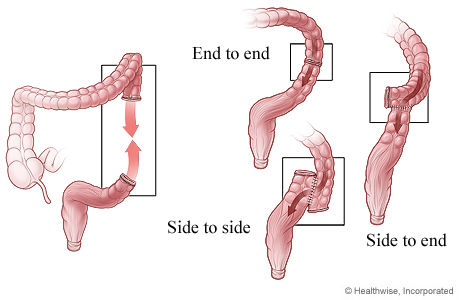
The process of intestinal resection surgery is carefully designed and precise. Surgeons make an incision in the abdomen to access the intestines. The affected section is removed, and the healthy ends are rejoined, a step known as anastomosis. This process ensures the digestive system continues to function.
Sometimes, special techniques like J-pouch or an ileoanal anastomosis are necessary. A J-pouch helps create a new storage space for waste if part of the colon is removed. In some cases, a coloanal anastomosis is performed, attaching the colon directly to the anus if the rectum is also removed. These techniques restore as much normal function as possible in intestinal resection surgery.
Medical Conditions Requiring Intestinal Resection
Various medical conditions necessitate intestinal resection. Intestinal resection surgery is common for gastrointestinal cancers. Removing the affected parts helps prevent the spread of cancer. Inflammatory bowel diseases, like Crohn’s disease and ulcerative colitis, sometimes don’t respond to medication, making surgery the best option.
Other conditions requiring intestinal resection include bowel ischemia, where blood flow is compromised, and bowel necrosis, where tissue dies. Issues like volvulus (a twisted bowel), hernias, and excessive scar tissue can all necessitate the removal of part of the intestine. These surgeries relieve symptoms and restore normal bowel function.
The Recovery Process After Intestinal Resection Surgery
Recovery from intestinal resection surgery varies but generally starts with a hospital stay of about five to seven days. Patients begin on a liquid diet, progressing to a regular diet as they heal.
Long-term recovery often involves lifestyle changes. Patients might need to adjust their activity levels and follow a specific diet. Consultation with a nutritionist can be beneficial for dietary adjustments ensuring adequate nutrition without overloading the digestive system post-surgery.
Remember, everyone heals differently. Some might bounce back quickly, while others need more time to adjust. Following the doctor’s and dietitian’s advice is crucial for a smooth recovery.
Potential Risks and Complications
Like any surgery, intestinal resection has potential risks. Complications can include an anastomotic leak where the joint between bowel ends is not sealed properly. Hernia formation is another possible complication, where a part of the intestine bulges through a weak spot in the abdominal muscles.
Adhesions, bands of scar tissue, are common after surgery, possibly leading to bowel obstruction. Short bowel syndrome can develop if a large section of the bowel is removed, resulting in nutrient absorption issues.
Understanding these risks and mitigating them with proper care is crucial. Attending follow-up appointments and promptly addressing any concerning symptoms can prevent complications.
Life With an Ostomy Post-Intestinal Resection
Certain intestinal resection surgeries might require an ostomy, where a stoma is created to allow waste to leave the body into a bag, bypassing part of the bowel. Ostomies can be temporary, allowing the bowel to heal, or permanent, if extensive bowel removal is necessary.
Living with an ostomy involves lifestyle adjustments. Learning proper stoma care is essential. Although it seems daunting at first, most people adapt well. Dispelling common misconceptions, like issues with scent or noise, helps ease the transition.
Preparing for Intestinal Resection: Key Questions To Ask
Before undergoing intestinal resection, preparing yourself with key questions is essential: – What should I expect post-surgery in terms of recovery? – Are there lifestyle changes I should anticipate? – How will this affect my daily routine and diet?
Discussing these with your healthcare provider enables you to strategize effectively and manage expectations. Adequate preparation ensures you have the support and resources needed for a smooth recovery.
Conclusion
Intestinal resection is a vital procedure that can greatly improve health. While the road to recovery requires time and patience, the outcomes can enhance life quality significantly. Support from healthcare professionals and loved ones ensures success through every stage.
Take the first step toward better health with expert care from Jiten Chowdhary. Trust our support and guidance throughout your intestinal resection journey for a smoother recovery and improved quality of life. Schedule your consultation today and start your path to wellness!